What is Patellofemoral Pain Syndrome?
Patellofemoral pain syndrome, common known as “runner’s knee” or “jumper’s knee”, is a condition where patient experiences pain in the front of the knee, around the kneecap, or patella. It is commonly found in people who are active in sports, especially females and young adults. Patient with patellofemoral pain syndrome will have difficulty performing day-to-day activities such as climbing stairs, kneel down and walking due to the pain and stiffness. In more severe cases, the gait pattern of the patient can alter and potentially leads to musculoskeletal pain in areas such as the ankle, pelvis and lower back.
What causes Patellofemoral Pain Syndrome?
 In most cases, patellofemoral pain syndrome develops when one engages in repetitive, vigorous physical activities such as squatting, climbing stairs and jogging. Furthermore, some alterations in physical activity such as increased frequency, intensity or duration of exercises each week might contribute to patellofemoral pain. Moreover, other factors such as rough playing surface and improper sports equipment or training technique might play a part in the development of patellofemoral pain syndrome.
In most cases, patellofemoral pain syndrome develops when one engages in repetitive, vigorous physical activities such as squatting, climbing stairs and jogging. Furthermore, some alterations in physical activity such as increased frequency, intensity or duration of exercises each week might contribute to patellofemoral pain. Moreover, other factors such as rough playing surface and improper sports equipment or training technique might play a part in the development of patellofemoral pain syndrome.
Other than physical activity, patellofemoral pain syndrome can also be caused by poor tracking of kneecap in the trochlear groove underneath it. This is called patellar malalignment and in this condition, the kneecap of the patient will shifts to either sides of the grove when the knee is bent. Eventually, the pressure between the back of kneecap and the grove will increase and irritate the soft tissues surrounding them, causing pain and stiffness. Patella malalignment can be caused by abnormal alignment of the legs between the hips and the ankles or weakness in muscles that attached to the knee cap.
Symptoms of patella femoral pain syndrome
Patients with patellofemoral pain syndrome usually feels a dull, aching pain around their kneecap. Other common symptoms include:
- Knee Pain during exercise and activities that repeatedly bend the knee, such as climbing stairs, running, jumping, or squatting.
- Knee Pain after sitting for a long period of time with your knees bent, such as one does in a movie theatre or when riding on an airplane.
- KneePain related to a change in activity level or intensity, playing surface, or equipment.
- Popping or crackling sounds in your knee when climbing stairs or when standing up after prolonged sitting.
Home Remedies
In most cases, patellofemoral pain syndrome can be improved with some simple home remedies. Patient could use the RICE method which stands for Rest, Ice, Compression and Elevation.
RICE Method
- Rest. Avoid putting weight on the painful knee.
- Ice. Use cold packs for 10 minutes at a time, several times a day. Do not apply ice directly on skin.
- Compression. To prevent additional swelling, lightly wrap the knee in an elastic bandage, leaving a hole in the area of the kneecap. Make sure that the bandage fits snugly and does not cause additional pain.
- Elevation. As often as possible, rest with your knee raised up higher than your heart.
However, if the pain persist, consultation with physical therapist or general practitioner will be recommended.
Treatment of patella femoral pain syndrome
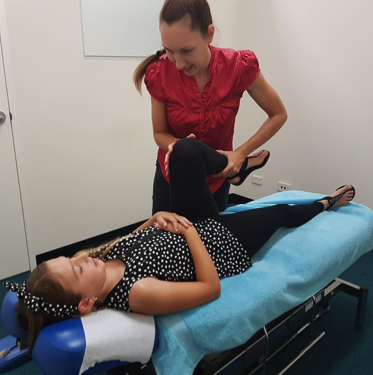 Patellofemoral pain syndrome can be treated nonsurgical. Physical therapist such as chiropractor may be beneficial as specific exercise that is tailored to the patient’s personal condition will be provided with the goal of improving the range of motion, strength and endurance of the patient. In most cases, exercise that focus on the quadriceps will highly recommended as those are the muscles that stabilise the kneecap.
Patellofemoral pain syndrome can be treated nonsurgical. Physical therapist such as chiropractor may be beneficial as specific exercise that is tailored to the patient’s personal condition will be provided with the goal of improving the range of motion, strength and endurance of the patient. In most cases, exercise that focus on the quadriceps will highly recommended as those are the muscles that stabilise the kneecap.
At Lakeside Chiropractic, our trained professionals will provide patients with exercise programme that is best suited for their conditions and we utilise low level laser technique that will help reduce any inflammation or irritation that might cause the pain. Lakeside chiropractic is located in Joondalup in Perth’s north and has visitors from many different suburbs including, Padbury, Kinross, Mindarie, Sorrento, Iluka, Carramar, Currambine, Tapping, Pearsall, Hocking and Woodvale. HICAPS Facilities available on site for major private health insurers (NIB, HCF, HBF, AHM, HCI and HIF) and also a part of the Medibank preferred practitioner and BUPA Members first network. If you would like to discuss any concerns, have any enquires or wish to book an appointment; feel free to contact one of our friendly staff on 9300 0095 or visit our website at www.lakesidechiro.com.au
References
https://www.edenprairiespine.com/blog/
https://orthoinfo.aaos.org/en/diseases--conditions/patellofemoral-pain-syndrome/
Dixit, S., Difiori, J. P., Burton, M., & Mines, B. (2007). Management of patellofemoral pain
syndrome. American family physician, 75(2), 194-202. (Physical therapy and taping of PFPS)
Petersen, W., Ellermann, A., Gösele-Koppenburg, A., Best, R., Rembitzki, I. V., Brüggemann, G. P., & Liebau, C. (2014). Patellofemoral pain syndrome. Knee surgery, sports traumatology, arthroscopy, 22(10), 2264-2274. (diagnoses and treatment of PFPS)
Thomeé, R., Augustsson, J., & Karlsson, J. (1999). Patellofemoral pain syndrome. Sports medicine, 28(4), 245-262. (diagnosis and treatment of PFPS)



